Plainly Put
New research explains how it does it
Doctors always warn against taking aspirin if you already have stomach problems, such as ulcers, and in fact prolonged aspirin use is discouraged generally.
I have often wondered about the mechanics of this, because in itself, aspirin is not a caustic substance, and never struck me as the direct agent causing the damage, A recent research paper has now shed light on the process and why this damage occurs.
Here is a summary of the key points from the research paper in plain language.
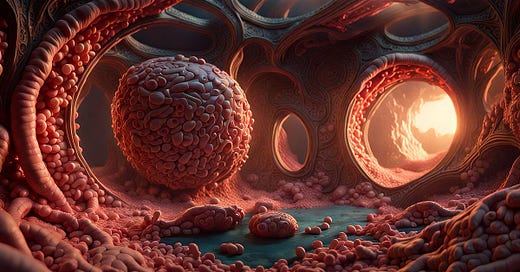
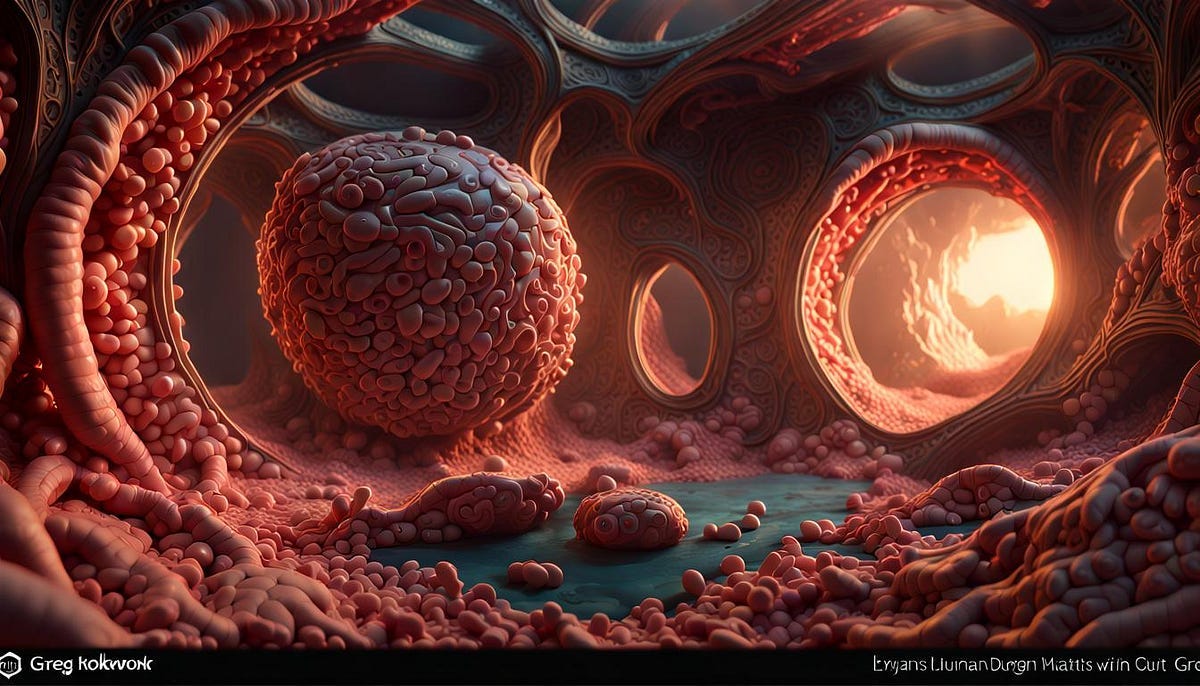
How Aspirin Harms the Gut
Aspirin can cause damage to the gastrointestinal (GI) system. New research found aspirin reduces good gut bacteria and bile acids, which hurts the intestine.
Aspirin Alters Gut Bacteria
Scientists studied people before and after taking aspirin daily for a month. Aspirin changed their gut microbiome — the community of microbes in the gut.
Specific bacteria called Parabacteroides goldsteinii were decreased the most. Studies in mice confirmed aspirin suppresses P. goldsteinii over time.
Aspirin Damages the Intestine
In mice, aspirin:
Thinned the intestinal lining
Reduced mucus-producing goblet cells
Decreased cell proliferation
Increased permeability
Caused bleeding
Increased cell death
Disrupted tight junctions between cells
This shows aspirin impairs the intestinal barrier. Mice with reduced P. goldsteinii had more severe damage.
P. goldsteinii Loss Mediates Harm
Mice treated with neomycin antibiotic also had less P. goldsteinii and more intestinal damage like aspirin.
But other antibiotics that didn’t reduce P. goldsteinii did not worsen aspirin’s effects as much.
Germ-free mice got no harm from aspirin until gut bacteria were restored.
Together this suggests aspirin’s impact on P. goldsteinii is key to the intestinal damage.
Aspirin Inhibits Bacterial Growth
Aspirin levels in the gut reached 1–4 mM. At these doses aspirin inhibited P. goldsteinii growth.
It interfered with the bacteria’s ability to make certain amino acids. Supplementing those amino acids reversed the growth inhibition.
P. goldsteinii Loss Alters Bile Acids
P. goldsteinii helps make a bile acid called 7-keto-LCA. Bile acids are important for gut health.
7-keto-LCA was substantially reduced by aspirin treatment. This contributed to the intestinal damage.
In summary then:
Aspirin suppresses P. goldsteinii bacteria and disrupts bile acid production, leading to harm of the intestinal lining.
Strategies to maintain P. goldsteinii may help protect the gut from aspirin’s effects.
Sources:
DOI: https://doi.org/10.1016/j.chom.2023.12.015
Creative Commons Attribution — NonCommercial — NoDerivs (CC BY-NC-ND 4.0) |